Vulvar Cancer
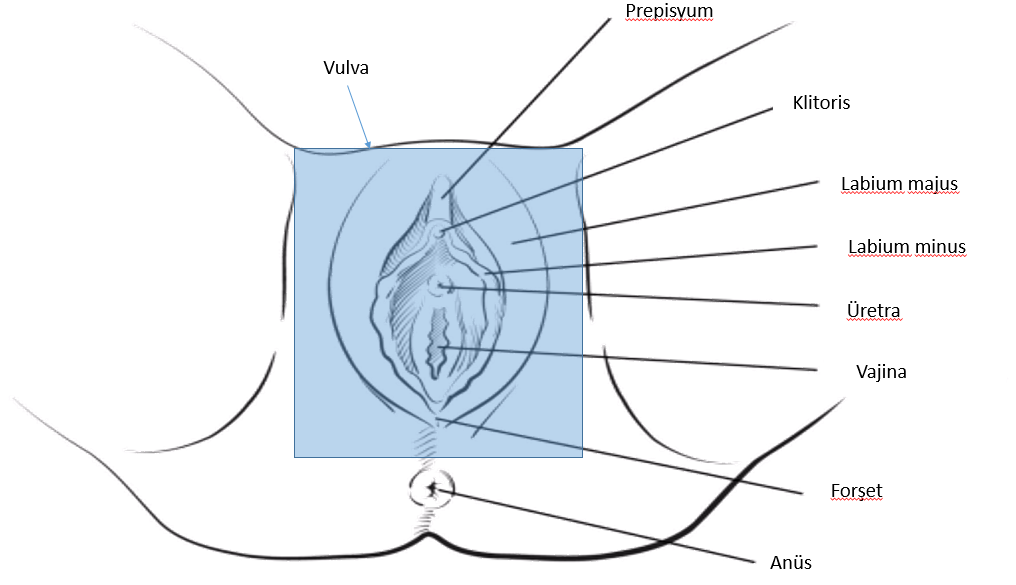
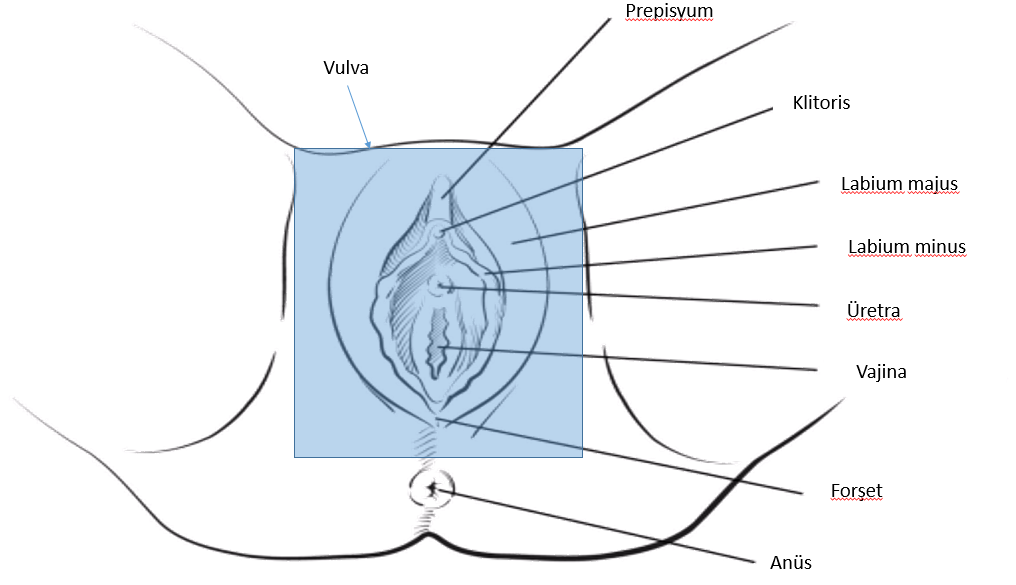
Vulvar cancer develops from the outermost part of the female genital organs. The vulva is the skin tissue surrounding the urethra, vagina, clitoris and labia.
Vulvar cancer usually develops as an itchy blister or wound. Although it is often seen in older women, it can also rarely occur in young people.
The treatment of vulvar cancer is surgery; the cancerous tissue and some healthy vulvar tissue are removed along with it. In some cases, the vulvar tissue can be completely removed. The earlier the cancer is caught, the less surgical intervention will be performed.
 Results
Results
- Persistent vulvar itching
- Pain and tenderness
- Bleeding that is not associated with menstruation
- Discoloration or thickening of the vulval skin
- Swelling, wart-like structure or open wound
When Should I Go to the Doctor?
If the above-mentioned symptoms have become persistent and concern you, I recommend making an appointment with your doctor. But let's not forget, it is the most rational way to have your regular gynecological examinations.
Reasons
Mutations that develop in the DNA of cells located in the vulva lead to the transformation of healthy cells into abnormal cells. Normal cells grow, multiply, and eventually die. Cancerous abnormal cells, on the other hand, grow, multiply uncontrollably and become immortal. This abnormal collection of cells forms a mass and it is called a tumor. Just as cancer cells can invade healthy tissues around them, they can also spread to distant tissues (metastasis).
Types of Vulvar Cancer
There are different types of vulvar cancer. The most common types are;
- Squamous cell vulvar cancer: This is the most common type. They arise from thin, flat cells on the surface of the vulva.< / li>
- Malignant melanoma: It is rare. They develop from pigment-producing cells in the vulvar skin.
Risk Factors
- Advanced age: Although vulvar cancer can occur at any age, it develops mostly in older women. The average age of occurrence is 65.< / li>
- Exposure to the HPV virus: HPV is a sexually transmitted virus that can lead to various cancers. Many women experience the HPV virus. In most of these women, the immune system destroys the virus, but in a small group of patients, cellular changes occur and the risk of cancer increases.< / li>
- Smoking
- The immune system is suppressed
- Precancerous lesions in the vulva: Vulvar intraepithelial neoplasia are lesions that develop in the vulva and increase the risk of cancer. Most patients do not progress to cancer. But a small group of patients may develop invasive cancer. For this reason, your doctor may recommend surgical removal of precancerous lesions.< / li>
- Skin disease found in the vulva: An itchy skin disease called lichen sclerosis increases the risk of vulvar cancer.< / li>
Protection
- Get information about the HPV vaccine from your doctor
- Have your routine pelvic exams
- Choose safe sex: Using condoms during intercourse reduces both HPV transmission and other sexually transmitted infections.< / li>
- Do not smoke: If you do not drink, do not start. If you have been drinking, stop immediately.< / li>
Diagnosis
- Examination of the vulva
- Colposcopic biopsy: Pathological evaluation is essential to confirm the diagnosis of cancer. The suspicious area on the vulva is examined with a special device called colposcopy, which allows it to be observed better by enlarging the tissues, and a biopsy is performed from this suspicious area. < / li>
Staging
If your doctor decides that you have vulvar cancer, he will want to conduct further tests to see if the cancer has spread to other organs. The stage of cancer is the most important factor that determines the treatment.
- Detailed examination of the pelvic area: To determine the spread of cancer, your doctor may perform a detailed examination of the pelvis and groin.< / li>
- Imaging tests: Advanced tests such as tomography, MRI, PET Sa-CT can be used to determine the spread of cancer.< / li>
Treatment
Surgery
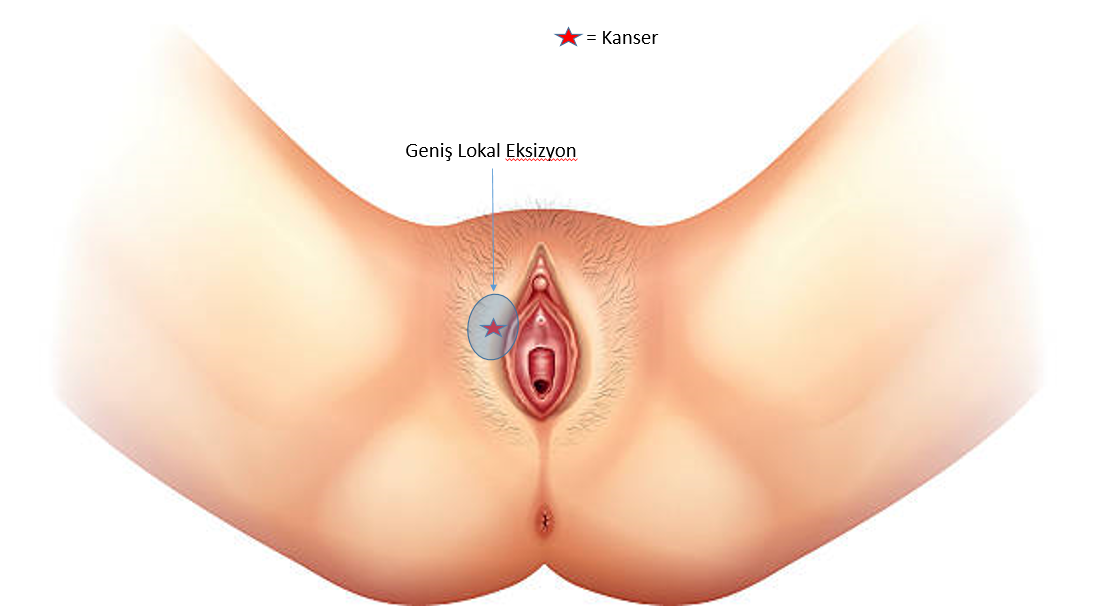
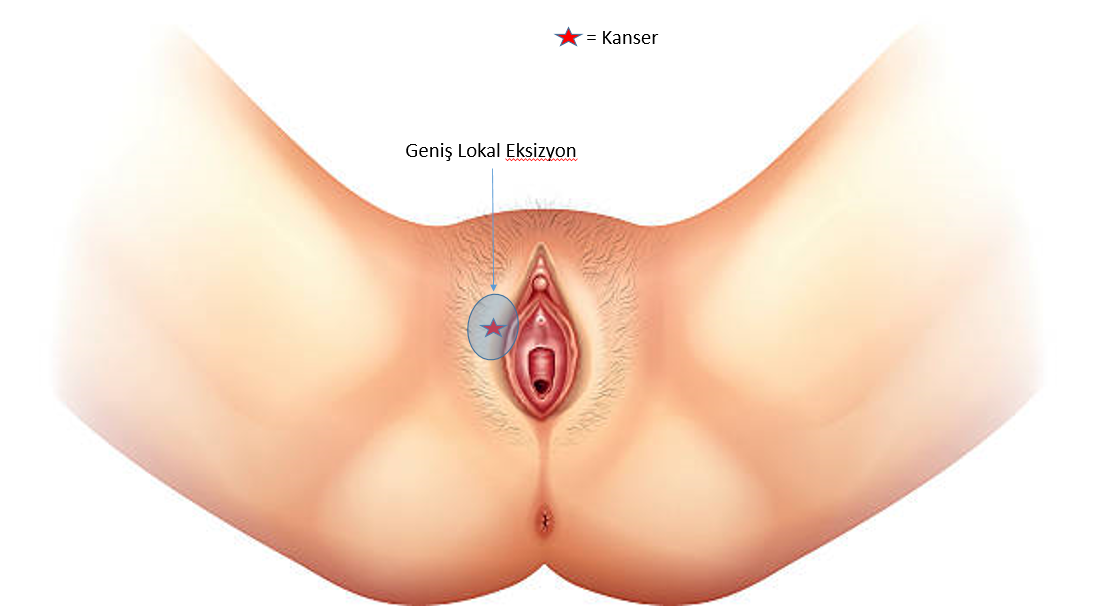
- Removal of cancer and some healthy tissue: This process is called extensive local excision and radical excision. A large tissue is removed, leaving a margin of safety in healthy tissues around the cancerous area. In this way, it is aimed to completely remove the cancerous tissue.< / li>
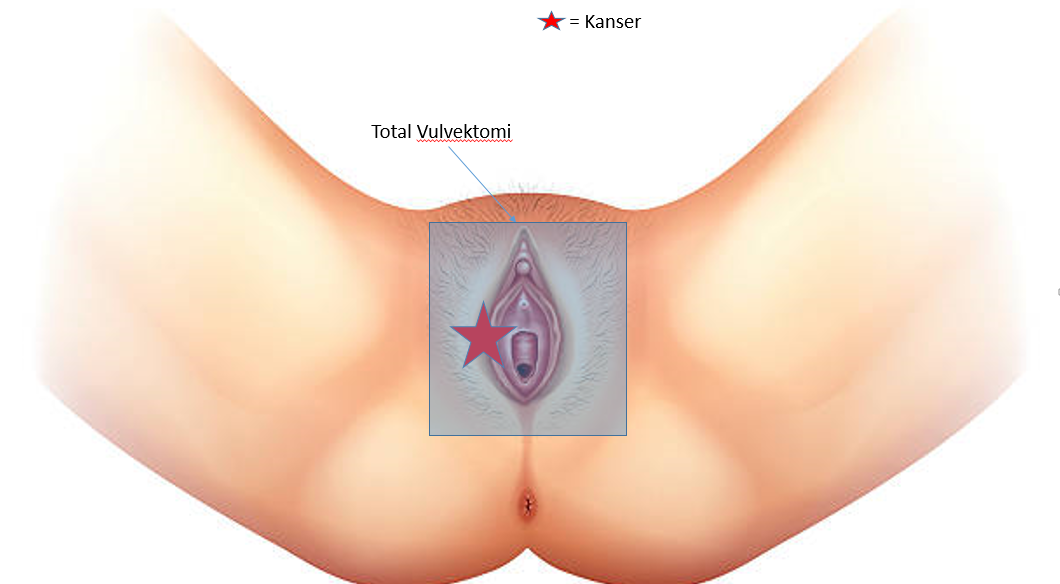
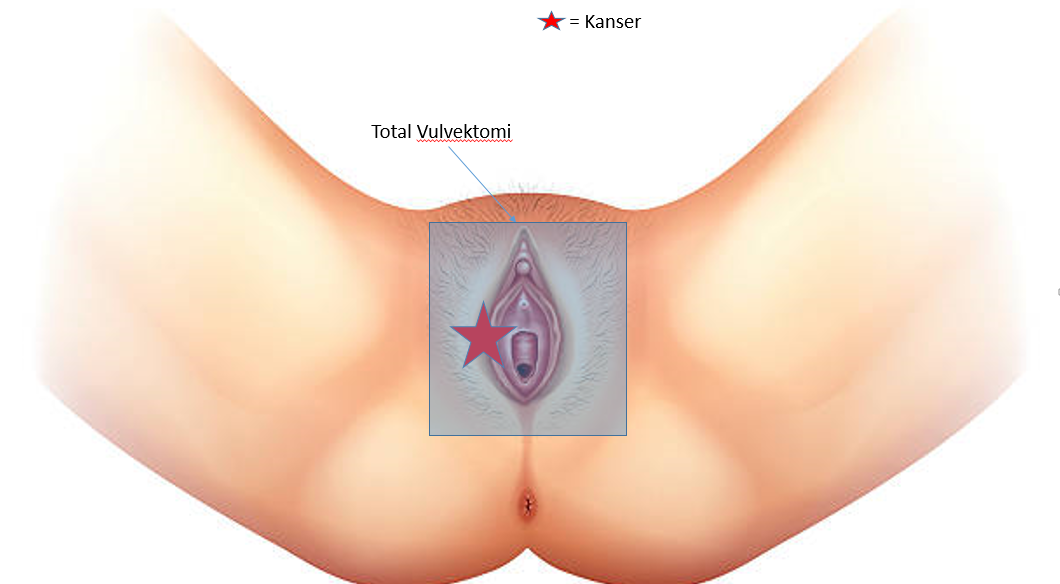
- Removal of part or all of the vulva: In extensive cancers, an operation can be performed in which one side of the vulva (partial vulvectomy) or all of it (radical vulvectomy) is removed along with the underlying tissues. Sometimes, the diameter of large tumors is reduced by radiation therapy and chemotherapy before and after surgery.< / li>

- Sampling of some of the lymph nodes (Sentinel node biopsy): By giving special dyes around the cancer, the lymph nodes that these dyes have stained in the groin area are removed. This procedure is called sentinel node biopsy. Thus, it can be understood whether there is a jump in the inguinal lymph nodes.< / li>
- Removal of many lymph nodes: If there are suspicious lymph nodes in the groin areas, all of them can be removed.< / li>
Radiation Therapy
Radiation is a special type of energy carried by waves and particles. The use of radiation produced in special devices in the treatment of cancer is called radiotherapy or radiation therapy.
It can be used to facilitate surgery by shrinking large tumors. It is sometimes used in combination with chemotherapy.
If there is metastasis in the inguinal lymph nodes, irradiation of this area may also be performed after surgery. In these cases, chemotherapy is often given along with it.
Chemotherapy
Special drugs are used in chemotherapy that destroy fast-growing cells. Cancer cells are also affected by chemotherapy because they grow fast. These medications can be given intravenously or orally.
If vulvar cancer has spread to distant organs, that is, if it is metastatic, chemotherapy may be preferred.
Summary
In cancer surgery the right surgeon, the right technology and the right pathology are essential. I strongly recommend that you research your surgeon, get opinions from patients he has operated on before, ask about the technologies that will be used in your surgery, and where and how the pathological examination will be performed.
 Results
Results